Digital health and healthcare priorities and trends. Prevention and care models in the age of digital transformation – collaboratively working towards a sustainable and inclusive prevention, care and post-care approach with people and outcomes first.
Digital health refers to the usage of digital technologies to enable universal healthcare access, improve healthcare quality/outcomes and enhance the health and physical and emotional well-being of populations.
The term digital health is rooted in eHealth, which is defined as the use of information and communications technology in support of health and health-related fields (WHO)
Digital health is a broad umbrella term that includes eHealth and the use of emerging and advanced technologies in the field of, among others, big data, genomics and artificial intelligence per the World Health Organization (more below). mHealth (mobile health) is a subset of eHealth while digital health is defined as the use of digital technologies for health, a field of practice for employing routine and innovative forms of information and communications technology to address health needs.
This WHO definition of digital health is not universal yet it’s good that it’s broad and introduces a common narrative and understanding. Digital health indeed needs to be seen as a broad concept whereby the purposes of healthcare are served through technologies that are combined for universal healthcare access, applications across various multi-disciplinary fields and ecosystems in healthcare and the health journey of people, as patients needing (access to) care and as citizens enabled to live healthier and prevent sickness (and thus the need for care).
While the digital technologies are a key component in digital health as enablers, they are not the goals. Myriad technologies, with data and the insights/actions they make possible (see big data, AI but also the Internet of Things etc.) are leveraged to improve both health and the efficiency of healthcare delivery, healthcare systems, healthcare facilities such as hospitals, work and life of healthcare professionals, healthcare innovation etc.
If digital technologies are to be sustained and integrated into health systems, they must be able to demonstrate long-term improvements over the traditional ways of delivering health services (Dr Soumya Swaminathan, Chief Scientist at WHO)
Health challenges and care system enhancements are increasingly addressed with a mix of digital health technologies across all levels of the complex ecosystem of ecosystems which healthcare in the broader sense is with its many stakeholders, from decision-makers in ministries of health and public health practitioners to the patients and all people involved in the actual delivery of healthcare.
Digital health and digital healthcare are the terms we use since many years to describe this broad set of technologies and most of all the purposes for which they are used.
They mainly revolve around the realization of a better healthcare through digital transformation that responds to changing needs and challenges on one hand and leverage new opportunities on the other by leveraging technologies.
While in the first place everything revolves around the patient (patient-centricity) and people as active participants in the prevention of diseases (the connected and engaged individual), there are several other stakeholders in this complex ecosystem.
It’s clear that healthcare workers in the broadest sense are key here. Digital health isn’t a replacement of healthcare, it’s an addition and, in the end, integration. Yet, the human aspect remains key in care, in the prevention of the need for care through education, involvement and programs on various levels and in any post-care stage or stage where less care is needed.
To understand what works and what doesn’t in digital health it’s key to take all stakeholders into account for the simple reason that without collaboration nothing works.
Digital healthcare, just as healthcare, is a highly connected given with multiple levels as such: policy makers and regulators; myriad participants in primary, secondary and tertiary care; the consumer/patient and his/her relatives; healthcare workers; administrators of healthcare facilities; the pharma industry; innovators in the digital healthcare space: the list is endless.
Just imagine all the people involved in the daily activities of healthcare facilities, for instance, and how healthcare facility management concerns complex ecosystems with multiple challenges and stakeholders as such but also with many different people needing access to the facility for literally dozens, if not hundreds, of possible reasons in their capacity as workers or visitors.
Improving healthcare quality and access while controlling costs as populations age, life expectancy increases and public expenditure on healthcare grows are a few of the main challenges for healthcare organizations across the globe.
Digital health – a holistic integration of technology-enabled enhancements in healthcare
Digital healthcare and all its segments, whether it’s mobile health (mHealth), telemedicine or telehealth, connected healthcare or any other term that’s been invented to describe forms of digital healthcare, are to be seen and evaluated from a holistic perspective and at the same time the individuals involved in healthcare, sooner or later all of us.
There is a lot of focus on technologies, applications and innovations in healthcare. It’s not always easy to understand what makes sense and what will prove to be a failure in an environment where commercial and financial interests are high, and some areas are hyped as digital healthcare and the application of technologies has accelerated in recent years due to emerging technologies that also create new possibilities through the sheer combination of possibilities these technologies result in.
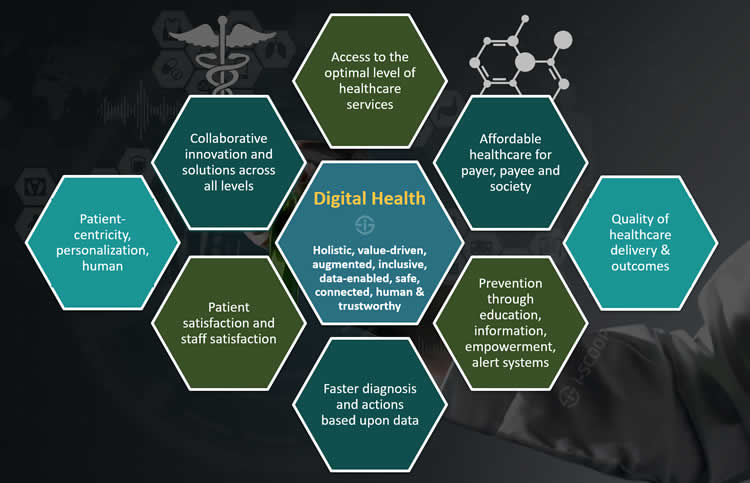
Yet healthcare isn’t the art and science of the potential; it’s what works that matters. The key goals of digital healthcare are, or at the very least, should include:
- Enabling affordable – universal – access to the best possible (“right” level of) healthcare (services) for all;
- Making the ways to achieve this goal, a.k.a. healthcare systems, sustainable and affordable for society (local, regional, national, supra-national), so for both healthcare payer, healthcare payee as well as for people involved in care who are still often overlooked;
- Educating and empowering people in a measurable way to prevent diseases, provide care when needed and activating circles of support;
- Enabling a faster diagnosis and insights/decisions based upon information to avoid far too many cases where speed could have made a critical decision;
- Putting people first: patients and their relatives, healthcare workers, anyone involved in prevention and care – technology should also be at their service, not the other way around;
- Bringing the various stakeholders in any healthcare system together to find collaborative and innovative ways to move beyond experiments and realize sustainable and effective solutions to address the changing and well-documented needs for healthcare today and in the future;
- Enhancing the quality of healthcare delivery and its outcomes;
- Improving patient-centricity in the full and true sense of the term, (which also means personalization and a recognition of the emotional and social factors since health as such is a holistic given) with a better patient satisfaction;
- Enhancing staff satisfaction: automation and digitization need to be truly enabling and augmenting capabilities and quality of work and interaction with patients;
- Enabling distributed and hybrid care delivery models whereby digital healthcare approaches allow to allocate resources, tasks and even the overall infrastructure including healthcare facilities. Coordination and exchanges between all stakeholders (professionals on various levels, professionals and patients in both directions) are essential to make this succeed;
- Developing innovative healthcare ecosystems with a place for new players and entities, including those that know how to position their often-digital offerings in an integrated multi-disciplinary approach that makes sense and respects the needs, behavior and demands of other partners, patients, healthcare payees and payers, and regulators.
- A digital transformation of healthcare that respects the key stakeholders, as well as their privacy and integrity, and that is bold enough to collaboratively gauge what is needed, what hasn’t worked, what is hype and what brings value, where change is needed to improve quality, availability and value of care, what needs to be stopped and what is worth replacing or adding from the vast landscape of digital healthcare evolutions – in a measured and as unbiased possible way, resisting pressure from interest groups that don’t want to see change happening where it is needed.
Obviously, technologies also play an essential role in the development of new treatments and means to help people with disabilities or chronic conditions, to name an important group, regain capabilities they might have lost.
Digital health: sticking to the essence with the principles of patient-centered care and the quadruple aim of healthcare
The list above is not exhaustive and some of the mentioned topics can be irrelevant or less relevant, depending on geography, healthcare system and other contextual factors.
You can of course add more and nicely categorize them according to one of various healthcare models or approaches such as the principles of patient-centered care or the good old quadruple aim of healthcare.
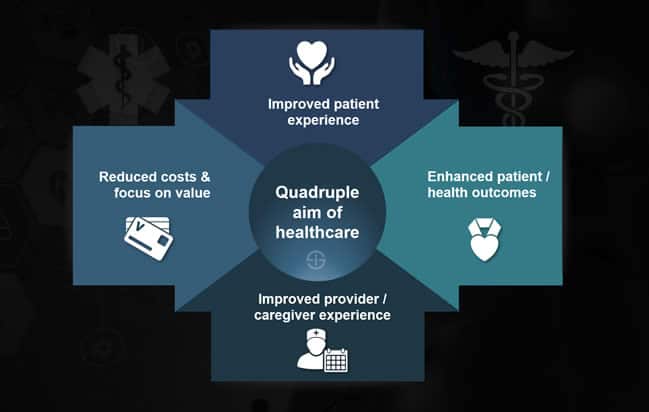
In case that’s new: in the nineties the Institute for Healthcare Improvement promoted a triple aim, revolving around the improvement of health, an enhanced patient experience and lower costs (there are variations and of course a more detailed explanation of key aspects per aim); the quadruple aim brought the work life of healthcare clinicians and staff into the equation: in a nutshell the idea was that enhanced healthcare worker satisfaction and improved patient satisfaction go hand in hand as is the case with employee satisfaction and customer satisfaction (and it was needed to focus on healthcare professionals).
So, simplifying that quadruple aim of healthcare consists of:
- Improving the patient experience;
- Enhancing health outcomes;
- Lowering the cost of care;
- Improving work life of providers: staff experience.
The digital health market: digital health is big business and only really starting
Since digital health is such a broad umbrella term and there admittedly is quite some hype regarding digital health whereby it’s often hard to distinguish between digital health applications and innovations that make sense, are endorsed by healthcare professionals and approved by the proper instances on one hand and myriad health applications that merely thrive thanks to the current hype on the other hand, gauging the value of the digital health market isn’t easy.
Increasing demand for remote monitoring services owing to rising incidences of chronic diseases worldwide is a major factor propelling the global digital health market growth (Global Market Insights)
It already starts with the definition of digital health since, despite the efforts of the WHO to come up with a shared language to describe the uses of digital technology for health with its 2018 classification of digital health interventions and 2019 recommendations on digital interventions for health system strengthening, obviously not all research firms use the same language.
Nevertheless, below are some forecasts about the value of the digital health market, immediately showing why so many companies have jumped on the bandwagon and there is somewhat of a hype.
According to Global Market Insights the global digital health market value is expected to surpass $504.4 Billion by 2025 of which USD 139.4 billion would go to the electronic health records business.
The illustration below shows some additional forecasts, compound annual growth rates and a look at the subsegment of mHealth technology. Overall compound annual growth rate (CAGR) per Global Market Insights is 29.6% with a higher CAGR for the mobile health segment.
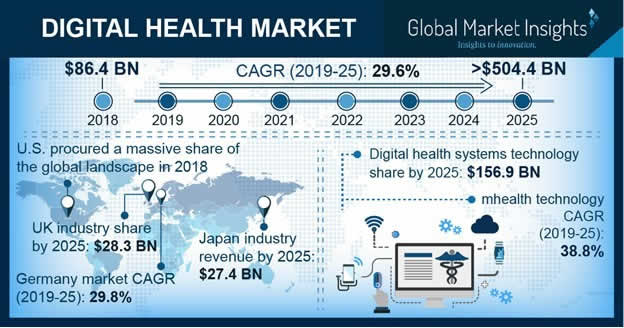
Transparency Market Research expects the market to be worth $536.6 Billion by 2025 while Grand View Research expects the market to reach $509.2 Billion.
So, all in all these few forecasts are relatively close to each other. P&S Intelligence, which defines digital health as referring to the integration of information technology into healthcare services with individuals, hospitals, and clinics being the end-users of digital healthcare solutions, equally expects huge growth for the digital health market which generated $73.1 Billion in 2017 according to the firm. Global Market Insights reports $86.4 Billion of revenues in 2018.
Digital health systems occupied the second largest revenue share in 2018 owing to rising government initiatives to promote digital health, resulting in an increased adoption of digital systems among healthcare systems (Grand View Research)
To show the difference between the digital health market and the healthcare IT market and how various research firms might use other definitions: while Global Market Insights expects the global digital health market value is expected to surpass $504.4 Billion by 2025, the same company expects healthcare IT market revenue to reach $441 Billion by the same year. Here, however, the electronic health record market is said to be expected to reach $97.8 Billion by 2025 which is lower than in the earlier mentioned forecast although it’s hard to tell what exactly has been incorporated in the data.
Note: in its digital health market announcement, P&S Intelligence stats that telemedicine, mHealth, electronic health records, and healthcare analytics are the various divisions of the technology segment of the domain. This would mean that some of the segments per the WHO definition of digital health might not be included. The links to the various report announcements above enable you to see the segmentation criteria the several research firms use.
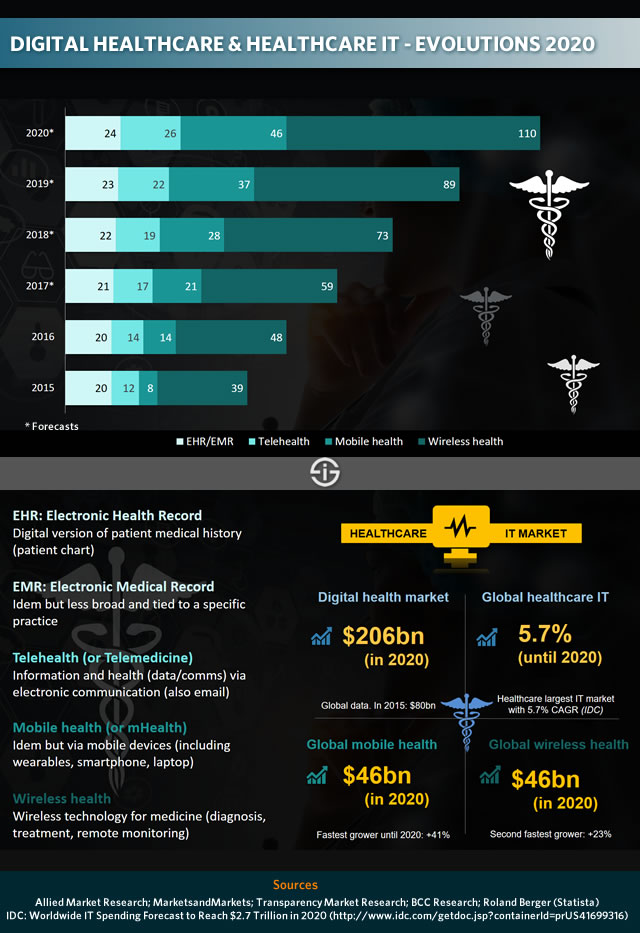
You might want to bookmark this page as additional data on the digital health market will be added, zooming in on the real important evolutions per region, segment, type of application and – to a certain extent – technology, in correlation with the main use cases across the healthcare ecosystem. Obviously it isn’t 2025 yet and forecasts tend to be reviewed so below are some older data that look at the market segments for 2020.
Digital health and healthcare IT
Below are some general trends regarding digital healthcare and healthcare IT with data and brief explainers per main categories.
Driven by rising consumer expectations, 60% of healthcare providers will make optimizing the digital patient experience a top 3 strategic imperative by 2020 (IDC, Top 10 Worldwide Health Industry 2019 Predictions)
You can also check out some of our older articles regarding the usage of healthcare technologies, for instance in the scope of the Internet of Things and healthcare. It’s clear that with the Internet of Things an important enabler of digital healthcare solutions has been added, not just in the sense of an additional major data source but also as an instrument to enhance the future of health on several levels in combination with other technologies. Already very present in applications for healthcare facilities and in prevention solutions consumers increasingly embrace, IoT opens up closer integration possibilities between clinicians and patients as well as means to make work life really easier for healthcare staff and enhance continuous care.
Without data and information, no digital healthcare evolutions can be realized. Learn more about the challenges, trends and opportunities regarding health information sharing, EHR and digital health records as the consumer/patient demands access to health data in our article on the 2019 FHI Index.
Digital health and the World Health Organization
As mentioned in the introduction and throughout this article the WHO has conducted – and is conducting – several efforts to classify the digital health reality and enable to speak a common language.
In April 2019, the WHO released a first guideline on digital health interventions, aimed at health policy-makers, government agencies and public health practitioners.
Digital health is not a silver bullet (Bernardo Mariano, WHO CIO)
The work builds further upon a classification of digital health interventions which revolves around the following key areas: clients, healthcare providers, health system managers and data services. This classification of digital health interventions or DHIs categorizes the ways in which technologies are leveraged to support health system needs and can be downloaded in PDF (also see the ‘poster’ below which you can equally download in PDF).
Pointing out that many digital health applications have been deployed without really carefully examining the evidence base on benefits and harms and that the enthusiasm for digital health has led to quite some short-lived implementations and an overwhelming diversity of digital tools, the WHO is clear with its guideline and “presents recommendations based on a critical evaluation of the evidence on emerging digital health interventions that are contributing to health system improvements, based on an assessment of the benefits, harms, acceptability, feasibility, resource use and equity considerations”.
This isn’t just important for healthcare and digital health overall, it also is an important instrument for innovative digital health start-ups that are more driven by highly valuable ways to enhance healthcare than perhaps the huge growth of spending in digital health.
The use of digital technologies offers new opportunities to improve people’s health. But the evidence also highlights challenges in the impact of some interventions. (Dr Soumya Swaminathan, Chief Scientist at WHO)
During a series of interviews which we’ve conducted with several healthcare professionals and innovators that work on highly valuable solutions in a collaboration between hospitals, universities/researchers, clients/patients and government agencies the concern to distinguish between yet another fitness or “me too” health app and professional applications was often voiced (more soon).
By way of an example: a mobile application (mHealth) that has been approved by the FDA and several other instances and healthcare specialists can be downloaded by consumers in the exact same app stores as applications that haven’t been developed in such a professional and valuable way at all. In some countries, efforts are done to build overviews of applications that really make a proven difference yet when it boils down to consumer-facing applications, app stores have far more leverage.
While this is just one of many examples regarding digital health, the following quote from the WHO guidelines on digital health does come to mind: “This guideline urges readers to recognize that digital health interventions are not a substitute for functioning health systems, and that there are significant limitations to what digital health is able to address…an understanding of which health system challenges can realistically be addressed by digital technologies, along with an assessment of the ecosystem’s ability to absorb such digital interventions, is thus needed to inform investments in digital health”.
As WHO Director-General Dr Tedros Adhanom Ghebreyesus puts in the WHO announcement: “Harnessing the power of digital technologies is essential for achieving universal health coverage. Ultimately, digital technologies are not ends in themselves; they are vital tools to promote health, keep the world safe, and serve the vulnerable”.
If digital technologies are to be sustained and integrated into health systems, they must be able to demonstrate long-term improvements over the traditional ways of delivering health services says Dr Soumya Swaminathan, Chief Scientist at WHO.
Digital health is a multi-disciplinary domain involving many stakeholders, including clinicians, researchers and scientists with a wide range of expertise in healthcare, engineering, social sciences, public health, health economics and data management
For example, the guideline points to the potential to improve stock management (one of the topics in a coming interview in our digital health series). Digital technologies enable health workers to communicate more efficiently on the status of commodity stocks and gaps the WHO states. “However, notification alone is not enough to improve commodity management; health systems also must respond and take action in a timely manner for replenishing needed commodities”.
More about the guideline that also make recommendations about telemedicine and emphasizes the importance of reaching vulnerable populations and ensuring that digital health does not endanger them in any way with some of the mentioned quotes and additional context in the WHO announcement and an executive summary of the guideline in PDF here.
Below is the mentioned poster with the classification of digital health interventions or DHIs from the WHO. Note: the guideline represents the first of many explorations into the use of digital technologies and has only covered a fraction of the many aspects of digital health the WHO reminds so stay tuned here as well.
More about digital health
Below are some of the mentioned interviews we conducted on digital health and additional articles and sources. This section is regularly updated with new interviews and data on digital health.
Telemedicine: complement or disruption?
For many telemedicine is an additional component to enhance healthcare delivery, quality of care, patient-centricity and the healthcare system as such through the usage of digital health technologies enabling to lower waiting times and lower costs, especially for low complexity care.
As the WHO says: digital health – and telemedicine – is a complement and won’t replace the system. Yet, not everyone agrees. For Prof. Dr. Leonard Witkamp, who is realistic enough to know that the health system now protects the system, telemedicine in the end will dramatically disrupt the way care is provided. Digital health as more than a complement indeed. According to Witkamp, many hospitals will go bankrupt if they don’t open their eyes and entirely review their models soon.
Read: “Telemedicine expert Leonard Witkamp on truly transforming the health system“.
Health records and information systems
Electronic health records or digital health records overall are the information backbone of digital health, at least in theory.
Ample interviews show a high dissatisfaction with the current systems that focus far too much on administration rather than on the patient journey. Not everyone agrees and the landscape does evolve. In the edition 2019 of its Future Health Index, Philips zoomed in on digital health records and information sharing, among other topics. The takeaway: there are shortcomings, overall respondents see benefits as well but there are quite some differences in the perceptions regarding today’s digital health records and information sharing, whereby there is a lack of information exchange between patient and clinician and not enough information exchange beyond the individual hospital or practice.
Read: “Future health: focus on health records and information sharing“
Digital health technologies in hospitals and healthcare facilities
The WHO classification of digital health interventions also covers health system managers and, within that scope, facility management with, among others the assessment of health facilities.
Yet, digital technologies also play an essential role in optimizing healthcare facilities, enhancing the patient experience and making work easier for healthcare professionals. Healthcare facility expert Chris Roberts looks at the changing face of healthcare facilities and how IoT, AI, machine learning and edge analytics, among others, enable to enhance operational efficiency, reduce the burden of administrative work and improve clinical workflows for clinical staff so they can spend more time with patients and optimize maintenance of equipment.
Read: “The future of healthcare facilities: collaboration and facility intelligence“
Digital health transformation: the hospital CEO perspective
Digital health encompasses various stakeholders with hospitals still playing a central role in most countries as we shift towards a more distributed form of care delivery.
The perspective of hospital CEOs is often somewhat different than that of eHealth pioneers. Nevertheless, they as well see that digital health is key for the future. In practice, however, there are other things to deal with to lay the foundations upon which hospitals can be part of a broader digital health transformation: common patient record systems, hospital networks, an intermediate level of care between home care and the hospitals with ambulatory care and so-called care hotels, automation of processes, digitization and so forth. While the technological innovations in many hospitals today revolve around the medical side of the equation – and continue to – hospital CEO Wouter De Ploey sees the larger and more impactful transformations coming in a second stage, once a certain maturity level is reached and the basis is there. Nevertheless, innovations are already part of the hospital sector at large.
Read: “Hospital network CEO Wouter De Ploey on automation and digital transformation in hospitals“
Other articles on digital health
Below are some more selected digital healthcare articles. More coming soon.
- mHealth: from research to real-life applications – interview Valerie Storms (Mobile Health Unit)
- Frank Dendas (Philips): new healthcare models have become a necessity
- The connected care market in North America
- Healthcare in digital transformation: digital and connected healthcare
- Electronic medical records – making data work for patient and clinician
- Internet of Things (IoT) in healthcare: benefits, use cases and evolutions
- Evolutions in healthcare and cybersecurity threats – go beyond compliance
- Information in healthcare: EHR success requires more than system adoption

