A look at the Future Health Index 2019 from the perspective of digital health records (DHR) and the impact of several information sharing and data-related update systems on the work of healthcare professionals, patient-related parameters and care quality/outcomes.
Healthcare challenges and enhancements are increasingly addressed with a mix of digital technologies across all levels of the complex ecosystem of ecosystems which healthcare in the broader sense is.
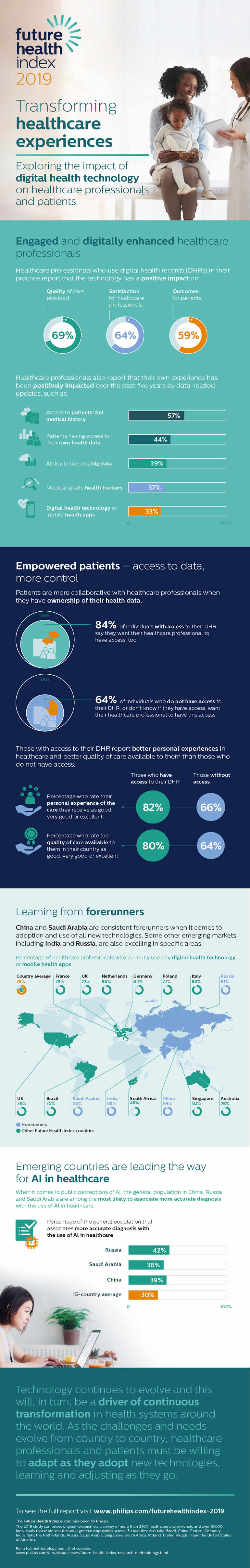
The possibility to leverage big data, have access to the full medical history of patients, to data from medical-grade health trackers and to digital healthcare technologies all contribute to the positive experiences of healthcare professionals- at least, to an extent.
The same goes for digital health records or DHRs according to the 2019 edition of the Future Health Index report, in which Philips tackles the role of digital health technology in enhancing clinician and patient experience.
Yet, while there are improvements and reported positive impacts regarding the usage of digital health data systems in the ongoing digital transformation of healthcare there are still ample shortcomings and a closer look shows important differences in perception concerning the impact of DHRs, with US healthcare professionals being least impressed by the impact of digital health records.
The Future Health Index report (the edition 2019 is the fourth edition) is based on a survey of 15,000 individuals (current and past patients) and over 3,100 healthcare professionals, which was conducted in 15 countries.
It offers a global view of healthcare developments and what is needed to accelerate the transformation of healthcare towards value-based care in future healthcare systems, including telemedicine.
On top of the experiences of both healthcare professionals and individuals (and the role/impact of digital health technology on these experiences), the Future Health Index this year also zooms in on those digital health records and on telehealth and artificial intelligence (mainly in relationship with the core ‘experiences’ theme). Future health is one of the topics at the 5th conference on digital health in September 2019 where Philips’ Frank Dendas is one of the speakers.
Data and experiences – the digital health record aspect in continuous care
Data and information are key in many of the report’s major takeaways, how else could it be?
As data and (health) information management professionals know, the word ‘right’ is important here and not just in the sense of the right information. The right access to the right level of care and right prevention at the right time through the right tools and right ecosystems of people and prevention/care entities is essential in future health developments. And the right data and information indeed is key to enable it.
The question is obviously what ‘right’ means and nowadays that’s a matter of patient-centricity, a more personal(ized) approach than ever and the means to map what is needed and effectively – collaboratively – realize the initiatives to meet those needs and ensure future health, keeping myriad challenges and developments into account. It’s clear that data is equally key for personalization.
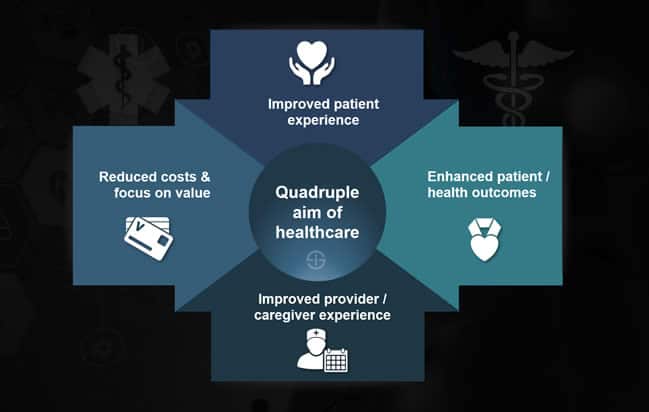
The Future Health Index 2019 report’s core theme, experiences of healthcare professionals and individuals, fits with two pillars of the so-called ‘quadruple aim’ of healthcare which Philips also has embraced for its strategic approach.
These in turn fit in the view of healthcare as a continuum (based on the continuous care model) which for Philips means connected care and health informatics enabling 1) healthy living, 2) prevention, 3) diagnosis, 4) treatment and 5) home care.
As mentioned in an article on the future of healthcare facilities, where ample technologies enabling to better leverage information such as big data analytics, artificial intelligence and the Internet of Things also have their place, the focus on improving patient experience and health outcomes or patient outcomes causes a shift to a more patient-centric model of care. Note, however: patient-centered care is about far more than digital health or even the patient experience.
All that said, time to look at some of those data-related findings and takeaways regarding digital health records.
How do ‘engaged and digitally enhanced healthcare professionals (increasingly) use digital health technology to improve their own experiences?
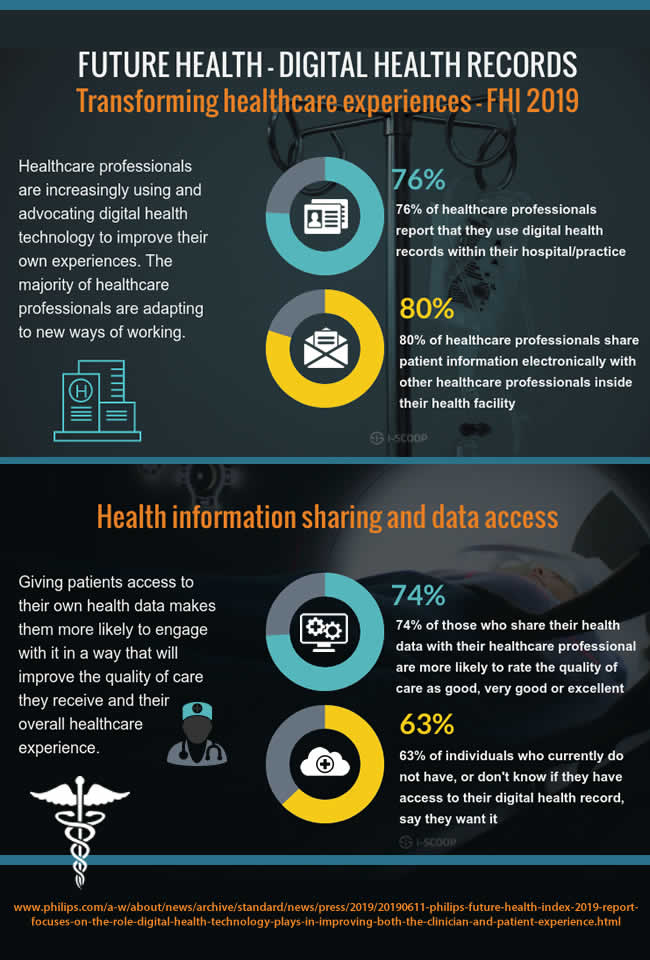
Philips’ Future Health Index 2019 found that the adoption and usage of digital health records or DHRs is growing. 76 percent of responding healthcare professionals say they use them within their hospital and/or practice, with 80 percent sharing patient information electronically with other healthcare professionals inside their health facility.
In case you’re familiar with the commonly used terms and practices of electronic health records (EHR) and electronic medical records (EMRs) you might wonder what digital healthcare records are since DHR is not really a universal term.
Philips defines DHRs as follows: “Digital health records can store a variety of health information, including medical history, test results, health indicators, etc. They can be used within a certain healthcare facility, across different healthcare facilities, by only the patient themselves, by one healthcare professional or across all healthcare professionals involved in a patient’s care”.
Some data from the Future Health Index on the adoption of DHRs and reported benefits:
- 69 percent of healthcare professionals using digital healthcare records in their practice, say that the ‘technology’ positively impacted the quality of provide care,
- 59 percent reports better outcomes for patients and;
- 64 percent sees a positive impact on healthcare professional satisfaction.
The future health report seems to indicate that, despite the complaints of doctors and other healthcare professionals regarding EHR (as part of DHR) with, among others, claims regarding an impact of EHR usage on physician burnout, serious EHR mistakes leading to legal cases in some countries, a negative impact of complex, monolithic and slow systems on healthcare staff and a resulting impact on actual quality time spent with the patient, all in all many healthcare professionals feel supported by DHRs even if the technology isn’t improving experiences for all. The latter is also what the authors of the future health report write. Yet, while the numbers don’t look too bad overall, let’s dive a bit deeper.
US and European healthcare professionals least impressed by impact of digital health records
When looking at the weighed responses per region an interesting picture emerges that tells a different story for the US and, to a lesser degree, several European countries.
As you can check yourself in the Future Health Index, edition 2019 (PDF opens) on page 27, there is a significant difference in the reported positive impact of digital health records per region indeed.
- In the US, 51 percent of responding professionals see a positive impact of DHRs on quality of care provided. The bad news: that percentage is the best of reported positive impacts concerning any of the impacted factors.
- Only 32 percent of US professionals see a positive impact of DHRs on healthcare professional satisfaction.
- Positive impact on patient outcomes is reported by 45 percent; on healthcare professional workload by 23 percent and on time spent with a patient by 25 percent.
- Finally, 36 percent reports a positive impact of DHRs on patient’s understanding of their health.

Philips recognizes that a lot of work is ahead in its Future Health Index 2019. Quote: “Many countries experience challenges with the implementation of digital health records and there is a common assumption that healthcare professionals feel these records can simply add administrative tasks to their workload”. With quite some systems and implementations this assumption has proven to be more than that.
Still, the authors of the future health report state that the research indicates that healthcare professionals recognize how DHRs can deliver on three of the four pillars of the Quadruple Aim with the previously reported overall reported benefits across all countries (so, not just US).
Moreover, 57% of healthcare professionals report that, in the past five years (which is a rather long period but also more or less corresponds with the buying cycle), their experience has been positively impacted by having access to patients’ full medical history according to the report.
The Future Health Index 2019 authors say that many healthcare professions are, however, still not seeing the benefits. This is no doubt the case: education, information and advocacy can be better in several areas. However, what’s also the case is that in some countries EHR has gotten a bad name among professionals for reasons we’ll tackle in that separate article.
In the European countries where the survey was conducted (France, Germany, Italy, Netherlands, Poland, Russia and the UK) the perceived positive impact of digital health records is better than in the US, especially regarding the quality of provided care.
Yet, other indicators are not what they should be either. Surprisingly, European respondents are even less positive about the impact of DHRs on patient’s understanding of their health than their US colleagues (31 percent compared to 36 percent). The second least positive impact for European professionals concerns time spent with a patient, followed by healthcare professionals’ workload.
Then where is positive impact highest? It seems that healthcare professionals from Brazil report the most positive impact of digital healthcare records on all parameters with the exception of (the reported positive impact on) healthcare professional workload where Asian countries seem more positive and of the impact on patients’ understanding of their health where healthcare professionals from these Asian countries (to be precise China, India, Saudi Arabia and Singapore) are far more positive (or Brazilians least positive) across all gauged impacted parameters.
The few Asian countries overall rank second regarding reported positive impact of DHRs, followed by APAC countries, being Australia and strangely enough – unless it’s a typo – again Singapore.
Jan Kimpen, Chief Medical Officer for Philips, on the digital healthcare records results: “While many conventional DHRs are often criticized by doctors because of their intrinsic shortcomings, it is encouraging to see that the FHI study shows that the majority of the doctors interviewed still find them useful, so that patient information is readily available to them and ready to share within their hospital”.
Sharing of patient information and the importance of data-related updates for future health
And that brings us to the sharing of information within the hospital or healthcare facility and with others in the broader ecosystem.
80 percent of healthcare professionals across all surveyed countries indeed share patient information electronically with other professionals inside their health facility. Sharing patient information electronically outside their health facility, however, is only done by 32 percent.
When looking at the reasons why healthcare professionals say they don’t share patient information with healthcare professionals inside and outside their health facility are:
- Lack of access to data-sharing systems;
- A preference of traditional ‘formats’ (phone, paper etc.);
- Concerns regarding data privacy and data security;
- Lack of interoperability of records systems.
The latter reason is the only one explicitly referring to EHRs and healthcare professionals won’t be surprised that interoperability is still an issue.
Healthcare professionals further report that their experience was positively impacted from data-related updates (or update systems, tools and capabilities) over the past five years.
In decreasing order of percentage of healthcare professionals reporting such a positive experience impact these include:
- Access to the full medical history of the patient with 57 percent of respondents.
- Access of patients themselves to their own health data with 44 percent.
- The ability to leverage big data (39 percent).
- Medical-grade health trackers (e.g., a connected glucose monitor; 37 percent).
- Digital health technology or mobile health apps, a broader category with 33 percent.
Unfortunately, except for Brazil and the US, we don’t have the results per country. It would, for example have been nice to see the results for Australia alone and certainly also for Europe where there are quite some differences between let’s say the UK, Poland and Russia regarding health systems.
Future health needs skills regarding data and communications techniques
EHR or not: the adoption of digital health records and their proper usage obviously isn’t just about systems but also about training and so forth.
Not all complex situations can be dealt with using simple solutions. Yet, simplicity and convenience will be key anyway. In the meantime, it’s training and knowing how to get the most out of the tools so the tools don’t eat the professional’s time and quality of work life but add to it (and to avoid errors with potentially grave consequences).
Healthcare professionals are rarely prepared in terms of how to use digital technology and data when they’re training for clinical practice. That’s what Patricia Mechael, Co-founder and Policy Lead at HealthEnabled and Technical Lead for the Global Digital Health Index, says.
“They may be receiving the latest information when it comes to clinical diagnostics and treatment, but they’re not being trained in the communications and data techniques that they’ll need to use alongside their clinical skills.”
Yet, there seems to be change. As the announcement of the Future Health Index 2019 puts it: “the majority of healthcare professionals are adapting to new ways of working”.
At the same time let’s not ignore the importance of their clinical skills and especially the need to really put the patient back in the center instead of spending too much time on screens as has been happening quite a bit in recent years. And one doesn’t need reports on physician burnout or issues with EHR and other systems regularly resulting in less ‘real patient time’. Unfortunately we need to go to doctors occasionally as well and, we’ll keep this for another time, let’s say interactions have somewhat changed, to put it mildly.
This brings us to the patient, data and digital health records, another topic in the Future Health Index 2019. Professionals/clinicians and patients can’t be separated of course.
Long before the patient experience became the key focus in digital health, the principles of true patient-centered care where established. Needless to say that communication skills are key here as well, although that doesn’t necessarily refer to the tools and techniques to communicate.
Although the positive impact of DHRs on healthcare professional satisfaction and other parameters is seen as low in some regions, we also need to point out the good and keep emphasizing the importance to leverage digital health records in a way that it doesn’t badly impact time spent with patients and quality of care to name just two.
Moreover, there is this important thing called collaboration or even symbiosis as Jan Kimpen calls it when saying that “The Future Health Index report highlights that health and healthcare is all about people. For example, the patient-clinician relationship is highly symbiotic. In terms of each party’s well-being, what one side does, affects the other and vice versa”. Very true. Again a reason to make sure that another partner in the relationship, the “system and screen”, doesn’t take too much place in bed as well.
The future health data tracking challenge in the relationship between individual and clinician
One of the other findings from the Future Health Index 2019 report concerns the usage of health trackers, in particular the sharing of data they generate by patients/consumers with clinicians recommending them.
It’s a well-known fact that all sorts of consumer-oriented health trackers are increasingly popular in times where people, given the proper motivation and social context, are more engaged and interested in monitoring, improving and checking their own health. Healthcare and fitness still lead the pack in the growing adoption of ample types of wearables and several other devices.
However, the tracking of health data, which can be done with connected devices of the consumer kind for specific health parameters but also with existing devices that are still predominantly sold in their non-connected forms for other parameters or with professional medical-grade trackers where needed, also plays a role in the relationship between healthcare professional and individual.
A relatively high number of healthcare professionals state that they encourage their patients to track health data. While approximately two-fifths of them recommend their patients to do so, only 9 percent of patients share the resulting data with them on a regular basis though.
All in all, this isn’t that problematic of course. The parameters the Future Health Index looked at are blood pressure, physical activity and weight (recommended to track by respectively 44, 42 and 39 percent of all responding healthcare professionals).
As can be expected ongoing exchanges of data concerning these indicators are rare and they happen more when issues arise (or when it’s time to see the physician again, if it’s done at all, as said still the exception). It’s a missed opportunity. When healthcare professionals never or very rarely get health indicator data from their patients they don’t have a complete view on their patients’ recent/current condition.
While ‘consumers’ show a higher interest in gaining access to their health data, within the context of trackers and beyond (access to digital health records as we’ll see below), there isn’t enough data sharing taking place the Future Health Index report concludes.
For Jan Kimpen two-way sharing of information is essential to deliver the right care at the right time and, as other results from the future health survey indicate, it also helps to improve the patient and clinician experience. Moreover, says Kimpen, informed and empowered patients take better care of their health – and that means a lower cost of care.
There is a case for the adoption of some cloud environment or other means of automated sharing, certainly for more vulnerable groups. One of the goals of specific forms of digital health tools is faster diagnosis and prevention. This is especially the case for specific conditions such as diabetes and sleep issues, to mention two. Blood pressure and weight, in combination with heart rate monitoring, lifestyle and medical history, can also help prevent, monitor and treat a range of cardiovascular diseases and chronic conditions.
The challenge for stakeholders in healthcare systems is how to organize it all. Who would the ‘consumer’ ideally share the data with? How is it all leveraged (sharing doesn’t equal checking or acting)? And there are of course also the devices and the motivations to share. Even financial motivations have proven to be less successful in this regard. Family, friends and personal relationships remain key here. In other words; again people.
The health-aware consumer might want to work closer together with the clinician regarding that data sharing to make the most of it. There are typically possibilities with several devices and vendors to build applications leveraging the data and enabling consumers to manage their health. And there are platforms in several markets enabling an exchange with a multidisciplinary or multi-level healthcare delivery ecosystem with ample initiatives in various countries. Sharing this data with care teams, clinicians or whomever else is key in the individual patient’s overall health is essential whenever there’s a case for it (and that case always exists) – unless the patient wants to be the healthcare professional or simply uses health data tracking apps and devices to stay or get in shape.
Future health – a matter of symbiosis and collaboration with data access as a driver
A last topic we look at that is stressed in the report (there are more as mentioned and as you can read here) is the empowered patient, in relationship with data and how access to it impact the patient-clinician collaboration.
You already know that the so-called connected, engaged and empowered patient is more demanding regarding the patient experience, the care version of the customer experience, is into the whole fitness, health and prevention phenomenon, wants convenience, choice and control, and wants access to health data.
Thinking back about the above-mentioned ‘symbiosis and the two-way communication access to data is part of the equation when aiming to realize a better collaboration between patient and healthcare professional.
As you can see in the infographic below, that also summarizes some other mentioned findings and additional ones that are tackled in depth in the Future Health Index report, ownership of their health data makes patients more collaborative.
84% of the general population with access to their digital health record say they want their healthcare professional to have access too while 64% of individuals who do not have access to their DHR, or don’t know if they have access, want their healthcare professional to have this access.
More importantly those who have access to their DHR report better quality of care and better patient experiences. Of the individuals surveyed, those who share their health data with their healthcare professional are more likely to rate the quality of care as good, very good or excellent (74 percent) compared to those who don’t share it (66 percent) the future care index announcement states.
“When patients are more involved in their care, anecdotally we do see better outcomes – they develop a richer and more sophisticated understanding of their health journey”, says Dr. K. Elizabeth Hawk, Clinical Instructor, Stanford University School of Medicine, Department of Radiology, Division of Nuclear Medicine; Radiologist, Matrix Division, Radiology Partners.
“Giving patients this access not only empowers them, it also builds a better relationship between physician and patient. And narrowing this disconnect can have a dramatic impact on physician burnout, too.”, Dr. K. Elizabeth Hawk adds.
And with physician burnout we’re again at one of the issues that are regularly cited in relationship with EHR, although the picture is more complex than that and one needs to look at the good of healthcare workers’ health and happiness from a holistic perspective, just as is the case with patients. Yet, as said, that’s for another article.
In the meantime, you can check out all results across various topics of the Future Health Index 2019 by downloading the report here. Some of the additional findings on other topics in the infographic below which you can download in PDF here.