Interview with Frank Dendas (Philips) on digital health, the transformation of the healthcare system, how technologies enable to enhance the four pillars of the quadruple aim of healthcare and what needs to be done for a sustainable care system.

Frank Dendas is Country Manager & Commercial Director Health Systems at Philips Belgium & Luxembourg. In this interview he shares his views on the digital transformation of healthcare at the occasion of an event on the topic.
In its recent Future Health Index report 2019, Philips reminded that, based upon the three previous editions of the study, it is hard for countries with a developed healthcare system to change, simply because of the legacy.
What about the healthcare system and future health in Belgium? We asked Frank Dendas about his views with a focus on his keynote at the event, entitled ‘The hospital without patients’ and elaborating on some of the key findings of the Future Health Index 2019 with the transformation of healthcare in the country in mind.

The point of care has shifted towards the patient – healthcare as a service
Let’s start with the topic of your presentation at the event. Can we see the notion of the ‘hospital without patients’ you will talk about in the context of a more ‘distributed’ view whereby hospitals are transforming as outpatient services, ambulant care become more important and care shifts closer to the so-called connected patient with, for instance, telemedicine and home care?
Frank Dendas: Many industries are being – or have been – disrupted, and healthcare is no exception.
Looking at other industries, we see that the companies causing disruption – or thriving amidst it – are the ones that successfully identified where the value for their end customer lies. In most cases, this means that they have boiled their offering down to a service – not a product. The Netflix versus Blockbuster example is a commonly known one, but the comparison still holds.
What I see as a “hospital without patients” is a healthcare center of excellence that has successfully identified the key value to their patients and has optimized their processes to deliver this in the most efficient way. At the end of the day, everybody that is active within healthcare wants to help people to live healthy lives and technology allows us to do so in new and innovative ways.
When a person has a health issue, what he or she wants, above all else is to understand what is wrong and to feel supported, helped and cared for every step of their healing journey. In many cases, this is not something that should be exclusively limited to within hospital walls – it is a service that can increasingly be offered at home.
The hospital without patients is a hospital that has managed to adapt to the patient as much as possible, and that requires as little adaption from the patient as possible. The point of care has shifted towards the patient.
The need for a healthcare system that promotes integration and collaboration
In that scope you will share concrete examples of how we can change patient pathways now. Can you share one with us or mention some of the ways that we can change patient pathways?
Frank Dendas: Without spoiling too much, I can already say that a lot is feasible today from a technological point of view.
Within Philips alone, we already have solutions that enable population health management, ‘first-time-right’ diagnosis, minimally invasive treatment and extramural recovery. This alone can already generate technologically advanced patient pathways that greatly reduce costs, while improving experience for patient and caregiver, as well as improving clinical outcomes.

It is equally remarkable that most of these solutions are already deployed in the Belgian healthcare system. They are however, deployed as point-solutions and often not as part of a seamlessly connected care flow.
Fundamentally, that is what is lacking today: a climate, a healthcare system, which truly stimulates and promotes the integration of all the technological innovation we are seeing.
To solve this, all healthcare actors need to come together and rethink the patient pathway. Only through collaboration, by looking at all the available puzzle pieces and at the playing field itself, can we deliver the seamless, patient-centric pathways and unlock the improved results for care providers, patients and the healthcare system. We believe that value-based healthcare is an essential component of this.
In this respect, my presentation is as much an invitation as it is a vision. We are not the solution, but we are convinced that we can be a part of it.
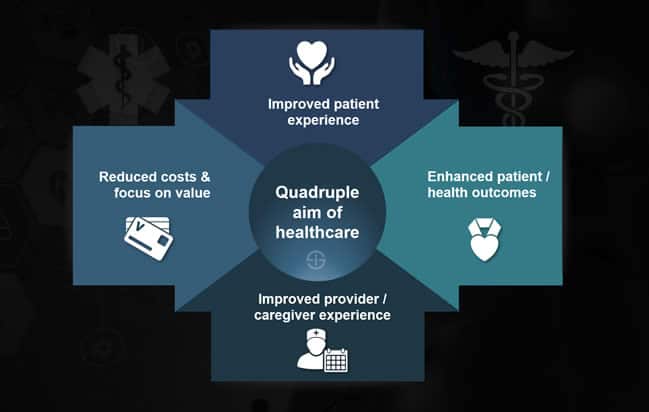
The quadruple aim of healthcare – the example of digital pathology
You will, among others, talk about ambulatory care or outpatient care to improve the operational and financial costs as well as health outcomes. These are among the so-called pillars of the Quadruple Aim of healthcare that is also central in Philips’ strategic vision. How does Philips enable enhancements across those four pillars? Can you give some examples?
Frank Dendas: For everything we do, the quadruple aim is the ultimate objective. When we say, ‘improving lives through meaningful innovation’, this is what we mean: any solution that at the same time reduces costs, improves outcomes, and improves patient experience and staff experience.
If a healthcare innovation does not deliver on one of these, it is not meaningful in the current climate.
Take digital pathology for instance – a solution that we have deployed in several hospitals across Belgium, with positive results. By digitizing the pathology department, we see that both patients and the treating specialists can get their results back a lot quicker. It goes without saying that within oncology, for instance, this is a massive improvement for both patient and caregiver, both in terms of outcomes and psychological well-being. At the same time pathologist also wins. These departments are often overwhelmed and by digitizing – or partially digitizing – their practice, they regain the time to focus on what is important.
I strongly feel that that is the essence of the quadruple aim: we deliver better outcomes and experience at lower cost, by digitizing what can be digitized and – this is the crucial part – in doing so, we offer breathing space to care professionals to truly focus on what is important and what matters most.
At the end of the day, care is a human activity. Technology is not there to replace caregivers; it is there to support them.
One of the other speakers at the event who specializes in telemedicine, Leonard Witkamp, says that by 2030 all big hospitals in The Netherlands will be bankrupt given, among others, high costs and the transformation of healthcare.
Frank Dendas: I am cautious with predictions, but we cannot ignore the fact that healthcare costs are increasing. As a result, new models are not just an option anymore, they have become a necessity.
I firmly believe that care is too important to be managed based on economics alone, but I am also convinced that in order to keep care affordable for as many people as possible, we need to look at it as a business.
The world is changing rapidly, and it is hard to predict what will happen even five years into the future. For the near future however, it seems almost certain that people will continue to age, and at times, get sick. It is our collective responsibility to ensure that when this happens, we have the infrastructure in place to address this in the best possible way.
Telemedicine and remote care in developed countries with a high population density
The adoption of telehealth and remote care is higher in countries where density of physicians is lower and/or there are regions where the physical distance between patient populations and caregivers is high. In countries such as Belgium and The Netherlands, density is high and distances very short. In more wealthy countries people are also used to relatively high-quality care, have more connected tools and are demanding too. How do these differences translate in practice?
Frank Dendas: There are different drivers for the adoption of telehealth and remote care. In the examples you mentioned – countries where physician density is low and the distances between patient and caregiver are often high – both telehealth and remote care are implemented as an immediate measure to increase accessibility of care.
While it is true that accessibility is not a concern for Belgium in this respect, for us telehealth and monitoring are a response to other challenges. Caregivers are under extreme pressure, and burnout numbers are high. On top of that, we are faced with an ageing population and more chronic diseases. By deploying remote care and telehealth, we can increase quality of care, while improving the experience for caregiver and doctor alike – all in a more financially sustainable way.
Because we still have a high-performant healthcare system, the need to deploy these solutions is less acute and the framework to deploy them in is often left to individual, forward-looking hospitals or caregivers. It is my conviction however that a successful deployment of these programs is needed sooner rather than later in order to keep the quality of care we have grown accustomed to affordable.
Digital healthcare records: information has been digitized but often the potential remains untapped
The edition 2019 of Philips’ Future Health Index zoomed in on three topics, including digital health records. Usage of digital health records seemed especially high in hospitals and practices of healthcare professionals. Yet, there is far less electronic sharing of patient information outside the health facility. Reasons include a lack of access to data-sharing systems, interoperability issues, security concerns and so forth. What challenges do you see in the Benelux? Is data sharing much of an issue here too?
Frank Dendas: Belgium has made impressive steps when it comes to digitization of healthcare – the fact that the eHealth plan, deployed by the government has achieved 72% of its 2013-2018 objectives is proof of this. A lot remains to be done however. Information has been digitized, but often its potential remains untapped.
A major challenge within Belgium is interoperability. In an ideal world, when I meet with a specialist – face to face or virtually – he or she should have seamless, highly secure access to my personal health data. This consists of all data I have captured and chosen to share, data collected by my general practitioner and my history in any hospital or care center. Through AI, an initial differential diagnosis is then provided, based on my symptoms and history.
We are not there yet. In Belgium very often digital records are often not compatible with one another – not just between hospitals or GPs, but sometimes within hospitals. In the interest of the patient, clear standards should be put in place. These can guarantee interoperability and security of data. That is not something any individual party can control, but this should be the result of a sector-wide agreement. At Philips, we make a very conscious effort to try to ensure that our solutions are designed in a way that ensures the as much compatibility and interoperability as possible.
Philips and healthcare: a holistic view of the health journey starts with prevention says Frank Dendas
If the role of hospitals changes and care is brought closer to the patient this must have an impact on the strategy of Philips as well since new solutions will probably to some extent replace some that are now more found in hospitals and healthcare facilities?
Frank Dendas: We have a very holistic outlook on health and more than one hundred years of experience in personal and professional healthcare. This puts us in a unique position in this industry.
We see that the line between patient and consumer is blurring and want to play an active role in making it easier for people to live healthier and more sustainable.
In terms of personal health, we want to continue to lower the threshold for healthy and sustainable level, in terms of professional healthcare; we want to continue to co-develop meaningful innovation that delivers against the quadruple aim, while also acting as a partner to hospitals and specialists when implementing these. As healthcare is becoming increasing value-based, we want to become the partner to maximize that value.
Earlier in 2019 you received an award whereby Philips was chosen as Best Brand for Small Domestic Appliances in Belgium. You mentioned that in the Benelux alone Philips helped improve the lives of 28.7 million people. What are the main types of applications in this context?
Frank Dendas: Here as well, it is important to emphasize that at Philips, we take a holistic view of people’s health journeys, starting with healthy living and prevention, precision diagnosis and personalized treatment, through to care in the home – where the cycle to healthy living begins again. We do not just want to “help people get better”; we want to help them live healthy for as long as possible.
The award we received earlier this year is an acknowledgement of these solutions. When it comes to domestic appliances, we create products that allow people to eat healthier with less effort (e.g. Airfryer, blenders, soup makers …), keep their homes healthy and clean (e.g. air purifiers, vacuum cleaners …) and track aspects of their own health (e.g. oral healthcare, mother and childcare ….). We see that consumers are becoming more and more digitized and engaged. Our products help to manage this evolution.
All of this aligns with the vision for a “hospital without patients” as well. If we empower people to live healthier and provide them with the tools to track their own health, then we can optimize the patient pathway once something does go wrong.
We feel that the line between consumer and patient is blurring and we want to play a role in lowering the threshold for a more prevention-oriented lifestyle.
Next in healthcare: Paul Stoffels (Johnson & Johnson) on global health challenges

