There are quite some hurdles that slow down digital transformation in healthcare. Many are non-technological in nature and, for example, include priorities, culture, and, inevitably, risks. While these hurdles exist in all industries that are digitally transforming, in healthcare, they are more complex and require more stakeholders to be involved.
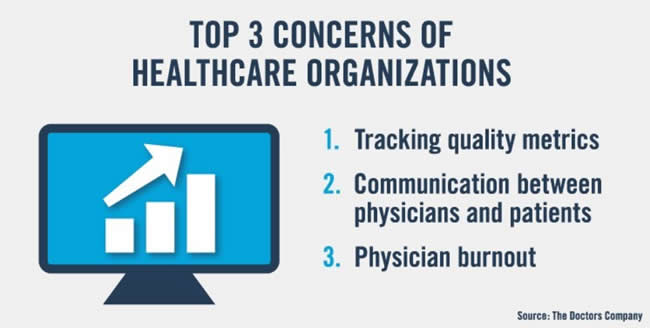
In fact, according to a survey, digital healthcare is a main concern for leading healthcare institutions in the US. Tracking quality metrics ranks first in the top 3 concerns of healthcare organizations, followed by communication between physicians and patients.
The latter jumped to the second spot of top concerns, before physician burnout, which still ranked second in the 2018 edition of the survey.
The two reported major technology risks in healthcare are respectively online media (same as in 2018) and electronic patient visits. With healthcare being the sector with most cybersecurity breaches, the main healthcare providers are also investing more resources in data security. Artificial intelligence is viewed as the main technology that could reduce risk.
The findings come from the 2019 edition of the Future of Healthcare Survey that was conducted by The Doctors Company. The results of the annual survey were unveiled early August 2019 at the Executive Advisory Board meeting, a US summit where almost 100 representatives of industry-leading healthcare organizations discuss some of the main issues in healthcare.
In interpreting the findings it’s obviously important to consider the US healthcare system and the activities of the organizers, The Doctors Company, which claims to be the largest physician-owned medical malpractice insurer in the US, with its 82,000 members.

Electronic health records behind most concerns of healthcare organizations
The legal aspect and focus on (reducing) risk as well as the malpractice link, are never far away. However, that’s the case with large healthcare institutions, including hospitals, across the globe anyway and electronic health records are related with that phenomenon in multiple ways.
As a hospital network CEO recently pointed out one of the reasons why such systems aren’t exactly what they should be yet is the fact that in acquiring and implementing them, compliance and liability are important factors, leading to the fact that they often are more a controlling system than a system that is geared toward supporting the care process itself.
Yet, at the same time the fact that EHR systems don’t serve healthcare professionals and patients, let alone the care journey, enough is precisely one of the reasons why there are still so many issues with them.
In the US the liability aspect is even higher. The reports and opinion pieces that call the implementation of EHRs a failure with grave consequences in the US had -quite some impact this year. It’s probably not a surprise that overall satisfaction regarding and perception of digital health records in the US is much lower than in other regions as mention in an overview of the 2019 Future Health Index from Philips. Most of the issues are well-documented and known but it’s clear that issues continue to exist.
What happened to making the data work for whom and what they should?
The problem is that in order to provide better quality care you obviously need data and in these days of big data and smart data and data everywhere that seems to be an even bigger concern.
In 2014, UK Professor Mike Pearson had a very simple yet still so relevant message regarding electronic medical records: “We need to create a purpose for each item of data collected. If there is no purpose, then don’t collect. Make the data collected work for the patient.”
Data needs to serve clinician and patient was his motto. Yet, already then, he pointed out that few solutions address the clinical interactions between clinician and patient in ways that both can agree enhance the outcome. Moreover, he didn’t feel as if developers and IT worked the way medicine does but rather the opposite.
Five years later we still hear similar comments with a few additions. One of them is the fact that, with the systems and the records and data, we have means to collect data as much as we want (and it does take quite some take to collect them for doctors and others using EHR systems as everyone knows).
Moreover, we do collect a lot. The question that remains is if ‘do we collect the right data and then actually do all the right things with it?’. Health economy Professor Dominique Vandijck for one doesn’t think so. Too much time is spent on measuring, not enough time is spent on improving he told us recently.
Yet, facts are what they are and the reasons why hospitals collect all possible data remain a matter of being ready in case of litigation. In the US, medical malpractice claims with allegations that the use of electronic health records contributed to patient injury or worse is on the rise since a few years. And the link with physician burnout has been made ample times too as you know.
In other words: it’s not surprising that there is quite some fear regarding digital health technologies and electronic patient records among US healthcare organizations. Still, if the US, as it does, wants to continue moving in the direction of integrated care with more ambulatory care, connected care, home care, telemedicine and mHealth applications added to the overall care picture in a way that makes sense, integrations/connections with systems enabling all these evolutions are key since, well, it’s about data in action in the end.
In fact, according to Professor Dominique Vandijck, health records are essential in an integrated healthcare approach. Yet one of the main challenges for those innovative connected care solutions that are growing fast in the US, is precisely that integration.
The same phenomenon can be seen elsewhere. mHealth expert Valerie Storms sees in daily practice how it stands in the way of healthcare innovation in even the most evidence-based types of solutions. Electronic health records, the issues concerning them and the reasons why they are needed (e.g. also for health economists and quality experts such as Vandijck) are a complicated matter indeed.
Talking about healthcare quality – and the parameters needed to measure it – it’s worth to repeat that tracking quality metrics, as is required by Centers for Medicaid and Medicare Services, continues to be the most important concern of healthcare organizations.
The challenge of communication between physician and patient
From EHR systems and quality metrics we jump to the second top concern of US healthcare organizations that’s inherently related with it: communication between physicians and patients.
While some digital health pundits think that soon technology will be an answer to everything, the relationship between physician and patient obviously remains critical and in that relationship communication is key.
The concern regarding these communications is related with the well-known fact that all kinds of administrative tasks and the usage of EHR systems takes time and in practice often more time than makes sense, even if considering all benefits and needs regarding data.
We all know the cartoons and, unfortunately indeed real circumstances, in which the physician looks at some screen and is busy with data-related work whereby the communication between both suffers. This too is a multi-faceted and complex issue. However, it would be too easy to blame it on digital health as such.
If there are too many tools, systems that are hard to use, compatibility issues and way too much data to collect, fields to enter and tasks to perform this also means that something is utterly wrong in terms of demands and the systems themselves.
This is in no way some defense of digital health since a lot in digital health will prove to be useless in the end too and it’s the care, the patient, the outcomes and the health worker’s experiences that matter. For sure, technologies play a key role in healthcare, certainly in the clinical aspect, but they’re not goals. And it seems clear that as things stand today even the goals for which some are used don’t entirely correspond – to put it mildly – with the goals for which they should be used or even have a negative impact on the goals of healthcare as they were.

And, yes, electronic health record systems are again mentioned explicitly as having a negative impact on communication. In the words of Richard E. Anderson, MD, FACP, chairman and CEO of The Doctors Company: “EHRs continue to have a negative impact on the doctor-patient communication”.
On the other hand, it can’t be ignored that the communication between physician and patient evolves and additional means of communication are added. As telemedicine expert Leonard Witkamp points out, in some countries, things like video consultations are being looked at, for instance because of a shortage of general practitioners.
Yet, all in all, everything that is ‘remote’, ‘tele’ or ‘mobile’ shouldn’t mean an end of communication either. In fact, as Valerie Storms reminded, mHealth applications don’t work without a clear communication. And all experts agree that, for any system to work, the exchange of information between patients and clinicians (and clinicians among them and with others such as specialists) are key in making this whole thing work.
Concerns with regards to the way people access healthcare: the impact of telemedicine, retail medicine and healthcare apps
Obviously, there are regulations and requirements that differ per country and region and, yes, digital communications, can be a concern from a security perspective as well – and obviously we need to keep in mind that The Doctors Company looks at the impact of everything on medical outcomes and malpractice litigation.
The two main technology risks in healthcare per the survey need to be seen from that perspective too, with online media such as websites and social media where accuracy of information, confidentiality and so forth join security. Electronic patient visits can be seen in a broader scope with other healthcare delivery evolutions.
Or, to quote Richard E. Anderson: “The concerns expressed by our nation’s healthcare leaders show the growing impact of digital healthcare…telemedicine, retail medicine, and healthcare apps are changing the way many people access healthcare. It remains to be seen how this will affect medical outcomes and malpractice litigation”.
That remains to be seen indeed. However, in a somewhat ideal integrated healthcare approach it wouldn’t just be about waiting and seeing but also about pro-actively steering and collaborating which will remain an ideal for a complex and large country since it already is for small ones.

In the meantime, the fact remains that, while digital health comes with benefits, leading healthcare organizations also fear it. And, in the survey, electronic health records are never far away in those top concerns or the factors behind them. Yet, no matter how you look at it, one thing is clear: people access healthcare differently with digital health. Just as Richard E. Anderson says.
Next in healthcare: Paul Stoffels (Johnson & Johnson) on global health challenges

