We are overflowing with data but, in my opinion, data without purpose says Professor Mike Pearson. An interview on the role of healthcare IT, electronic medical records and what digital health applications should enable for patients and clinicians alike.
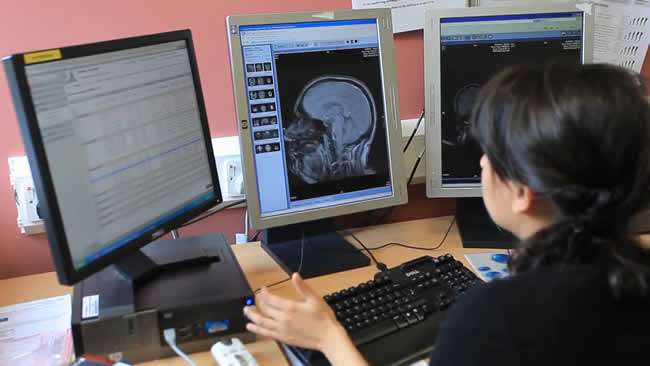
Aintree University Hospital is one of the largest hospitals in the UK and a pioneer in moving from paper based medical records to an intelligent, electronic medical records approach. Professor Mike Pearson was consultant physician at Aintree University Hospital NHS Foundation Trust.
Tom Herbst interviewed Professor Pearson on the role of IT, electronic medical records and the information challenges in healthcare and technology in 2014. His advice remains highly valuable for anyone wanting to enhance patient care, develop solutions that both patients and healthcare professionals want and, last but not least, leveraging big data and analytics for the patient’s well-being and patient experience.
Most healthcare software is designed by people who never had a patient interaction
Earlier this month, The King’s Fund released the final report of the Commission on the Future of Health and Social Care in England. It shows there are hard choices to make. The system is not coordinated, and the impact of the ageing population proves to be a significant increase of the percentage of GDP spent on health and social care. How can IT help in solving healthcare challenges?
Professor Mike Pearson: There is no doubt that IT in various forms can improve the efficiency and effectiveness of any system and healthcare is no exception. BUT of the many apps/programs/packages out there, few so far address the clinical interactions between clinician and patient in ways that both can agree enhance the outcome. And even fewer make use of the data collected within the apps to feed back information in ways that makes the task of practicing medicine more productive and enjoyable.
Most software is designed in offices by people who have never had a patient interaction. This is the key challenge to solve – get IT to work the way medicine does and not the other way around.
Digitization and electronic medical records: more than scanning paper records
You spoke at the International Digital Health and Care Congress of the King’s Fund. Can you tell us a bit more about your presentation?
Professor Mike Pearson: I was talking about how Aintree University Hospital addressed and solved its legacy paper records challenge to free up space, improve clinical and operational productivity and ultimately enhance patient care. Our award-winning system cost us £1.5 m and we’re saving £1 m each year not shuffling paper around our system.
Self-evidently paper records are bulky, clumsy to move around, slow to sort through to find details and all too often get mislaid or lost. And the handling and storage costs of people and buildings is huge.
Scanning such paper into a digital file solves all this. BUT the scanned record must be logically laid out FOR THE CLINICIAN, searchable for commonly used forms and results, and the searching must be faster than for the paper predecessor. A year on with all records scanned, our hospital would not go back – and the millions saved is being used for direct patient care.
The theme of the event was “improving health through the use of technology”. How can technology help in solving the challenges we’re facing according to the Barker Commission (Commission on the Future of Health and Social Care in England) report?
Professor Mike Pearson: Electronic storage is hugely cheaper than the paper equivalent. It is also more accessible and much more secure too. But there is so much more that could be done with the information that is stored electronically if only the algorithms could be devised. The sort of algorithmic issues that will make most difference are those that influence the clinical decision making and to write them requires clinical brains to set out the clinical issues in yes/no flow charts so that the computer programs can get to work.
There are few clinicians who are trained or familiar with the needs of the programmer and even fewer programmers who understand the nuances of medicine.
We need to create a purpose for each item of data collected. If there is no purpose, then don’t collect. Make the data collected work for the patient.
Electronic health records and healthcare data: on exceptions and purpose
Also in September, IDC organized its Healthcare Summit in London. While research showed an uptake in the adoption of EHR (Electronic Healthcare Record) systems, the annual rate at which the global EHR market is forecasted to grow, is only 5.5%. What are your thoughts?
Professor Mike Pearson: Medicine combines both art and science. Most disease situations have exceptions and thus most decisions are taken on a balance of probabilities and the tipping point varies according to the risks involved and the views of the patient. Indeed, the most logical treatments can be rejected by patients and that right must be respected. The art of adjusting the aims of therapy to suit the situation while also accounting for patient views means that most algorithms start off simple but end up with so many branches that the package becomes too difficult to use. And of course, if an exception is overlooked there can be disastrous consequences for a patient.
An example: a patient is referred up as end stage cancer to hospital. The consultant looks at the patient and X-rays and “something” nonspecific does not quite fit.
It’s based on a feeling (so not quantifiable) and by next day a completely different diagnosis and outcome emerges. How can one code for clinical experience that comes from having seen something like that before? It is possible of course but not easy.
BUT using medical knowledge to focus on the most important pieces of information can make it possible to design systems that can be practical as well as clinically safe.
An often-heard message at the IDC event was the need to disjoint data from apps to manage the data deluge in healthcare data. What is your take on that?
Professor Mike Pearson: We are overflowing with data but, in my opinion, data without purpose. It’s rather like having 500 different ingredients that might be used to bake a cake. Put in all 500 and all you have is a mess. Instead we need to define the 5 needed for a victoria sponge – harvest those 5 – and you have an edible cake. So, we need to define the purpose for each data collection i.e what will make a difference for specific patients or specific situations.

Focusing on the financial and clinical benefits equals a winning electronic medical records implementation
In 2013 Aintree University Hospital NHS Foundation Trust won the public sector project of the year award in the Computer Weekly European User Awards for Enterprise Software.
Used by around 3,000 health professionals on a daily basis, the Trust has stopped using paper health records in clinical practice and installed an electronic document management system from CCube Solutions, along with custom portal to provide clinicians an electronic medical record.
George Lawrie, vice-president and principal analyst, application development and delivery, Forrester Research, who was on the judging panel with other experts from research firms such as IDC and Ovum added: “We were impressed by Aintree University Hospital NHS Foundation Trust’s focus on the benefits, both financial and clinical, of the solution.”
Aintree was the first NHS Trust to successfully work with a third party – Capita Total Document Solution – using a scan-on-demand approach to outsource the huge task of scanning its records library.
Professor Mike Pearson commented: “Some Trusts have just scanned the whole patient record which is useless as doctors are presented with thousands of PDF pages and accessing information is almost impossible. The innovative indexing system developed for our solution means notes are always available and we can find many results as quickly or faster than using paper.”
Professor Mike Pearson and Ward Priestman, director of informatics, both from Aintree University Hospital NHS Trust, talk about the project in the video below.

